Already updated since first posting!!!
So many acronyms…
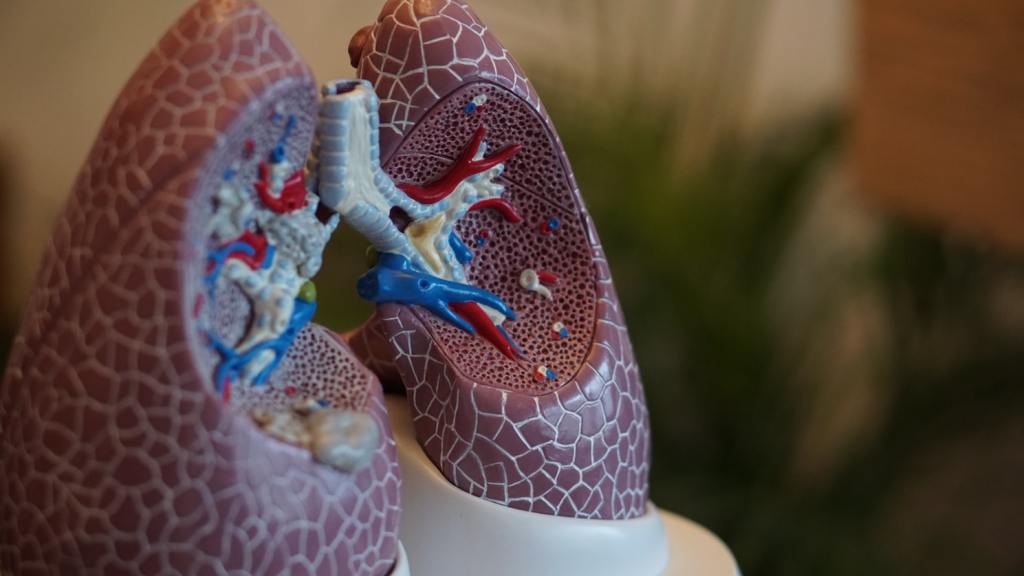
Non-Invasive Ventilation (NIV) and Non-Invasive Positive Pressure Ventilation (NIPPV) are some of the more advanced respiratory interventions being provided to some patients who experience COVID-related and non-COVID-related ARDS. These interventions are pretty much what they sound like: mechanical ventilation is provided to the patient with or without positive pressure without the process of intubation to maintain the airway.
This advanced intervention is utilized in patients where ARDS has not progressed to the severe stage, but the patient is not progressing or stabilizing on just supplemental oxygen alone. This may seem WAY OUT OF YOUR LEAGUE. But its not! PTs in other countries are providing support to their respiratory and physician colleagues by providing these interventions to patients. If your interest is piquing, Italy is leading the way.
Some states, like Michigan, have opened up the scope of practice lines to allow PTs to function essentially as respiratory therapist extenders, where we can provide advanced respiratory interventions under the guidance of our more familiar interprofessional colleagues. There are, of course, some PTs who are probably more familiar than others, but for those that are not, you can do this with help. Even though I currently practice and reside in Texas, I am from Michigan, as are many of my colleagues. I hope this blog is helping some of you up there!

So, for NIV, pressurized air with supplemental oxygen is provided both during inspiration and exhalation. Typically, during exhalation there is little to no pressure. The goal of this is to support the patient’s natural inspiratory efforts and decrease the work of breathing, but a small amount of PEEP may be provided. NIV should also reduce the need for intubation if it is successful at stabilizing ventilation and diffusion. NIV can be used acutely (such as in the case of COVID-19 and other ARDS generating conditions like COPD exacerbations), but can also be used chronically, similar to a CPAP.
As you can see in the picture, a nasal mask can be used, but you can also provide NIV via nose/mouth mask, face shield, or even a helmet! There are several different options for machinery that can provide this support. The difference between a CPAP and NIV (also known more commonly as BiPAP) is that CPAP provides a single expiratory and inspiratory pressure, whereas NIV provides differing inspiratory and expiratory pressures.
There are contraindications and relative considerations for use of NIV, so please do your research. Active ventilator-associated pneumonia or undrained pneumothorax are good reasons to stay away. However, I know with COVID-19, at some point it comes down to a risk/benefit analysis with risk being death and benefit being maybe less death. If successful, there is decreased mortality with this intervention in comparison to mechanical invasive ventilation.
NIV and COVID-19
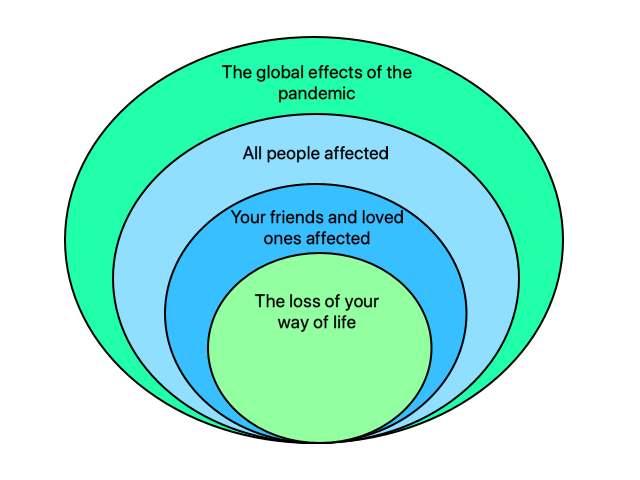
We need this in COVID-19 because the damage to the pneumocytes in the lungs due to viral overload may prevent diffusion of CO2 from the blood stream to the alveoli, preventing CO2 removal. Poor oxygen diffusion happens simultaneously due to the same alveolar destruction. Therefore, respiratory support efforts are needed for BOTH inspiration (IPAP) and exhalation (EPAP) which results in BiPAP.
We have talked in previous posts about methods of hyperinflation that can be used to recruit under-inflated airways such as glossopharygeal breathing. The purpose of using NIV is basically the same. Keep airways open and improve gas exchange. More oxygen in AND more CO2 out.
We have also talked about providing positive expiratory pressure using different devices and techniques to increase small airway expansion and inflation for the exact same reasons. NIV can be modified to allow for the addition of positive pressure to achieve these exact same things. This is called NIPPV. This intervention can be provided at the same time as supplemental oxygen and airway support and decreased effort of breathing. Man, I’m really wishing I had one of these in my trunk right about now for all those home care visits!
So the whole point of all of this is to reduce need for invasive ventilation because of the demand it places on the medical unit and it’s personnel as well as the detriment it can result in for the patient. According to many docs and RTs, it’s succeeding!

Most of you have seen CPAP or BiPAP machines so don’t be intimidated. I used to futz around with mine all the time. They are typically set at a certain pressure setting (or settings if BiPAP) and they can’t be modified without a RT or a physician making changes via a computer system. So you really can’t screw it up. In the acute care setting, you will probably have a lot more access, so take care and consult your team.
Here is a great video on how to set up NIV, in case you need a crash course.
This is such a great opportunity to reclaim some of our practice that we gave so little focus to prior to this pandemic. As this is my favorite practice area, I’m excited for the opportunity and I hope you are, too!
Respiratory therapists are out there literally saving lives and I love the chance to help them do that! Tell me about your favorite experience working with a Respiratory Therapist in the comments!

Follow @DoctorBthePT on Twitter for regular updates!